August 26, 2012 Annual Meeting Highlights

Sunday
On Sunday, the 30th ASRS Annual Meeting featured the:
- AMD I Symposium
- PAT Survey presentation
- Macular Surgery I Symposium
- Imaging Symposium
- Retinal Vascular Symposium
Retina Image Bank: Image of the Day
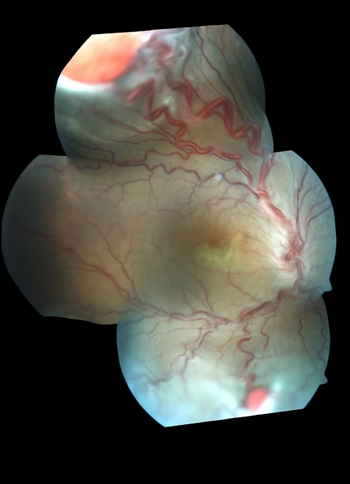
Condition: Von Hippel-Lindau disease
Photographer: Gabriela Lopezcarasa Hdz. Hospital Angeles Lomas
Imaging device: Fundus cameras, FF4
Description: 29-year-old woman with decrease in visual acuity secondary to serous retinal detachment in Von Hippel-Lindau disease
AMD I Symposium
Sunday, August 26, 7:35-9:37 AM
Moderators: David Williams, MD, MBA, Pravin Dugel, MD
Reported by Polly Quiram, MD, PhD
Minneapolis, Minnesota
Systemic Complement Inhibition With Eculizumab for the Treatment of Geograhic Atrophy in AMD: The COMPLETE Study
Presenters: Zohar Yehoshua, MD, MHA, and Philip Rosenfeld, MD, PhD
Moderators: David Williams, MD, MBA, and Pravin Dugel, MD
COMPLETE study results show systemic complement inhibition with eculizumab (Soliris - anti C5 ab) does NOT slow the progression of dry AMD nor reduce drusen volume.
Baseline Predictors of Visual Outcomes and Treatment Frequency in Patients With Wet Age-Related Macular Degeneration (AMD) in the First Year of HARBOR
Presenter: Brandon Busbee, MD
Predictors of visual outcomes in patients with wet AMD in first year of Harbor showed better outcomes with a younger age of presentation, lower vision at baseline, and smaller area of leakage.
A predictor of fewer injections in patients with wet AMD in first year of Harbor was the presence of less than 118 microns of subretinal fluid at baseline.
Early OCT Responses at Day 7 and Month 1 Post Ranibizumab That Predict Visual Acuity Outcomes and Injection Frequency at Month 12 in the HARBOR Study
Presenter: SriniVas Sadda, MD
Eyes with SRF day 7 after the initial injection of ranibizumab show better gains in BCVA compared to eyes without significant SRF.
Retinal Pigment Epithelial Cell Loss in Patients With Neovascular Age-Related Macular Degeneration
Presenter: Richard Spaide, MD
RPE cell loss in wet AMD (determined by absence of autofluorescence) is associated with duration of disease and prior PDT. RPE cell loss occurs in greater than 50% of eyes and is not similar to GA; it starts centrally and is multifocal.
Correlation of Retinal Morphology and Visual Acuity in the Comparison of Age-Related Macular Degeneration Treatments Trial (CATT)
Presenter: Glenn Jaffe, MD
CATT results showed significant change in lesion composition (decrease in fluid and increase in fibrosis) following treatment with anti-VEGF agent. Vision decrease was associated with persistent intraretinal fluid and presence of fibrosis.
Flexible Macular Capillary Recruitment in Relative Hypoxia as a Homeostatic Adaptation With Pathologic Implications
Presenter: Joseph Maguire, MD, MBA
Macular capillary recruitment is an adaptive mechanism that occurs during states of relative hypoxia. Changes in retinal anatomy associated with macular diseases may induce long-term recruitment that plays a role in macular diseases (RAP lesions, telangectasias, collateral formation and CR anastamoses).
PAT Survey Presentation
Presenter: J. Michael Jumper, MD
PAT Survey Editor
The ASRS Preferences and Trends (PAT) Survey had 631 respondents this year, a 65% increase over the 2011 survey. Trending data was presented for several medical and surgical questions that have been asked over the years. Also, the response rate was large enough to compare answers of US/Canadian members with those of International members.
Interesting findings from this year's survey include:
- 10.8% of US/Canadian respondents now report that they would use Eylea as first- line therapy for subfoveal CNV due to AMD.
- In an effort to reduce endophthalmitis risk during intravitreal injection, 63% of US/Canadian members state they "avoid talking and ask the patient not to speak," whereas 46% of international respondents "wear a mask and ask the patient not to speak."
- 67% of US/Canadian respondents follow a treat-and-extend protocol in the management of wet AMD, whereas International members see patients monthly and treat as needed.
- 46% of respondents state that they also peel ILM during vitrectomy for epiretinal membrane "76%-100%" of the time.
Macular Surgery I Symposium
Sunday, August 26, 1:15-3:10 PM
Moderators: Mathew MacCumber, MD, Baruch Kuppermann, MD, PhD
Reported by Judy Kim, MD
Milwaukee, Wisconsin
"Foveal Red Spot," "Macular Microhole" and "Foveal Photoreceptor Defect" in the Era of High-Resolution Optical Coherence Tomography
Presenter: Edward Hall, MD
Accurate nomenclature is needed to categorize outer foveal defects. Dr. Hall suggested that the term "macular microhole" (MM) should be reserved for small, full-thickness macular holes between 50 to 150 microns.
The term "foveal photoreceptor defect" should be used for what was previously called "foveal red spot" (FRS). These have focal foveal outer photoreceptor layer defect and may be observed in a number of disorders such as macular telangiectasia. Dr. Hall and colleagues concluded that clinical and spectral domain OCT examinations allow for anatomically accurate nomenclature and classification.
Surgical Outcomes of Macular Holes Associated With Idiopathic Macular Telangiectasia
Presenter: Judy Kim, MD
Eyes with macular telangiectasia (MacTel) type2 can develop full-thickness macular holes (FTMH). There is limited data on surgical outcomes of these eyes. Dr. Kim presented a case series of FTMHs that developed in the setting of MacTel Type2 and reviewed the literature. She showed that the hole closure rate following surgical intervention is quite low in MacTel eyes compared to the highly successful surgical outcomes in typical idiopathic FTMHs.
Dr. Kim suggested that it may be due to the underlying pathogenesis of MacTel Type2 with neurodegenerative changes resulting in loss of Muller cells. She stressed that it is important to recognize that some FTMHs may have developed in association with MacTel, since these eyes have poorer surgical outcomes than idiopathic FTMHs.
Vitrectomy Outcomes for Lamellar Macular Holes Associated With Epiretinal Membranes
Presenter: John Thompson, MD
Dr. Thompson evaluated the outcomes of vitrectomy for lamellar macular holes secondary to epiretinal membranes with reduced visual acuity in 55 eyes. The mean preoperative visual acuity (VA) was 20/100 and the mean postoperative VA was 20/63 (P = .003) at 1 year and 20/50+2 (P < .001) at 2 years. There was a mean VA gain of 2.2 lines with 40% of eyes achieving 20/40 or better.
VA improved 2 or more lines in 49.1% and decreased 2 or more lines in 10.9%. Causes of decreased vision included development of choroidal neovascularization (3.6%), recurrent epiretinal membrane (3.6%) and visually significant cataract (3.6%). He found no difference in VA gain between eyes that had ILM removed with ICG vs no ILM removal. Dr. Thompson concluded that vitrectomy is an option to improve VA in visually significant lamellar holes associated with epiretinal membranes.
Outcomes and Predictive Factors in Bilateral Macular Holes
Presenter: Emmanuel Chang, MD, PhD
Dr. Chang and colleagues performed a retrospective study of all patients who underwent bilateral macular hole surgery between 1985 and 2011. The incidence of bilateral macular holes was 3.1% with a 3:1 female-to-male ratio. Approximately 1/3 of patients had asymptomatic vitreomacular traction in the opposite eye on initial presentation with macular hole on OCT that eventually progressed to a macular hole.
Surgical closure rate with first surgery using ICG-assisted ILM peeling was 94%; 7% of operated eyes developed recurrent macular holes with a median of 1.2 years during a mean follow-up of 5.1 years. Strongest predictor of visual acuity outcome was the hole duration being less than 6 months and the stage of hole did not appear to affect visual outcome. The authors concluded that the outcomes of bilateral macular holes are excellent with ICG-assisted ILM peeling technique.
Ocriplasmin for the Treatment of Patients With VMT and Full-Thickness Macular Hole: Subgroup Responder Analyses from the Phase III MIVI-TRUST Program
Moderators: Suber Huang, MD, MBA, John Thompson, MD
Presenter: Carl Regillo, MD, FACS
Dr. Regillo presented the data from 2 Phase III clinical trials comparing a single intravitreal injection of 125 µg (100 µL) of ocriplasmin to a single (100 µL) placebo injection for the resolution of symptomatic vitreomacular adhesion (VMA) with primary outcome at Day 28. He described subgroup analyses evaluating vitreomacular traction (VMT) release without epiretinal membrane (ERM) and nonsurgical closure of full-thickness macular hole (FTMH).
At Day 28, 56/188 (29.8%) ocriplasmin subjects with VMT had resolution of VMA, compared with 6/78 (7.7%) of placebo subjects. The VMA resolution rate in VMT patients with an adhesion of < 1500 µm was higher than for those with broader adhesion of > 1500 µm. By Day 28, 40.6% of the ocriplasmin-treated patients demonstrated nonsurgical FTMH closure compared to 10.6% (P < .001) with placebo. Resolution of these conditions resulted in clinically significant VA improvements.
Ocriplasmin Single Intravitreal Injection for the Resolution of Symptomatic Vitreomacular Adhesion Including Macular Hole: MIVI-TRUST Safety Findings
Presenter: Baruch Kuppermann, MD, PhD
Dr. Kuppermann presented the safety data from MIVI-TRUST clinical trial. The most commonly reported ocular adverse events occurring > 5% incidence and more commonly than placebo included vitreous floaters, photopsia, and blurred vision. Fewer retinal tears and detachments were observed in ocriplasmin patients vs placebo patients with 1.6% vs 2.7%.
Safety findings for ocriplasmin patients included reduced VA (0.7%), dyschromatopsia (1.0%), ERG changes (0.2%), dyschromotopsia and ERG changes (1%). He concluded that ocriplasmin was well-tolerated. Dr. Kupperman also concluded that ocriplasmin has a favorable safety profile and allows for a minimally invasive pharmacologic treatment for patients with vitreomacular traction and full-thickness macular holes.
Imaging Symposium
Sunday, August 26, 3:40-4:36 PM
Moderators: SriniVas Sadda, MD, Jay Duker, MD
Reported by Robert Wong, MD
Austin, Texas
Acute Macular Neuroretinopathy (AMN): New Insights into Diagnosis, Natural History and Pathogenesis as Revealed by Sequential Multimodal Imaging EndFragment
Presenter: David Sarraf, MD
Dr. Sarraff presented a case series of 8 patients of acute macular neuroretinopathy reporting the structural and functional changes as these lesions evolve over time. Using Fourier domain OCT, infrared and autofluorescent images, he showed that IS/OS defects resolve, but OS/RPE defects and ONL thinning may persist and these lesions may be associated with corresponding visual field defects.
Preclinical Evaluation and Intraoperative Human Retinal Imaging With a Microscope-Integrated Spectral Domain Optical Coherence Tomography Device
Presenter: Paul Hahn, MD
Dr. Hahn presented updates on a novel device to provide real-time, high-resolution intraoperative OCT images using a microscope-integrated OCT (MIOCT) during vitreoretinal surgery. He reported > 80% correlations between MIOCT and handheld OCT data on eyes with macular pathology.
PIONEER: A Prospective Intraoperative and Perioperative OCT Study-6-Month Vitreoretinal Results
Presenter: Justis Ehlers, MD
Dr. Ehlers presented intraoperative handheld and perioperative OCT during vitreoretinal surgery data in the PIONEER trial involving 49 subjects. Novel findings include increased hyporeflectivity under IS/OS line after membrane peeling as well as other subclinical alterations in foveal architecture.
Does Spectral Domain OCT Provide Any Additional Information to Non-mydriatic Fundus Photography Screening?
Presenter: Rishi Singh, MD
Dr. Singh presented 568 patients who were screened with non-mydriatric fundus images and SD-OCT at a primary care setting and the additional OCT images rarely refuted the original diagnosis (12%). The largest benefit was SD-OCT's ability to pick up ERM and VMT better than fundus photography.
Functional Retinal Imaging with Triple-Wavelength Imaging Reflectometry (TIR)
Presenter: Kristie Lin, MD
Triple-wavelength imaging reflectometry (TIR) can estimate the amount of rhodopsin in the retina in vivo and this may be helpful in assessing photoreceptor function in patients with macular conditions like AMD. Further investigation of this technology may identify this to be an important biomarker of disease progression.
Microglia in Retina: Can We See Them In Vivo?
Presenter: Gennady Landa, MD
Analysis of the inner plexiform layer (IPL) reflectivity on SD-OCT images may indirectly evaluate the status of microglial cells which may correlate with macular diseases. Interestingly, conditions such as geographic atrophy and retinitis pigmentosa, typically thought of primarily outer retinal diseases, exhibit IPL lower reflectivity. Further investigation is warranted.
Retinal Vascular Symposium
Sunday, August 26, 4:36-5:42 PM
Moderators: Jeff Heier, MD; John Pollack, MD
Reported by Asheesh Tewari, MD
Detroit, Michigan
Increased Vision With QLT091001 in Blindness Due to Mutations in RPE65 or LRAT Genes
Presenter: David Saperstein, MD
There is rapid and significant improvement in visual function parameters after a 7-day course of QLT091001 (an oral cis-retinoid prodrug) in patients with early-onset retinitis pigmentosa (with mutations in LRAT or RPE65). This drug is not vitamin A.
Macular Telangiectasia Type 2: Is It a Vascular or Degenerative Disease?
Presenter: Emily Chew, MD
Macular telangiectasia Type 2 is more of a degenerative than a vascular disease, based on OCT findings and histopathology of Mueller cell loss.
Intravitreal Aflibercept Injection in Central Retinal Vein Occlusion: Results of the Phase 3 COPERNICUS Study
Presenter: David Boyer, MD
Intravitreal aflibercept given monthly (2mg) for macular edema due to CRVO had improvement of vision. It was well-tolerated and had a favorable safety profile.
Time to Clinically Significant Visual Acuity Gains Following Ranibizumab Treatment for Retinal Vein Occlusion: BRAVO and CRUISE Trials
Presenter: Allen Thach, MD
Ranibizumab treatment of macular edema from BRVO and CRVO can result in significant visual acuity gain from baseline.
Anti-VEGF Therapy Significantly Reduces the Rate of Neovascular Glaucoma Due to Central Retinal Vein Occlusion
Presenter: Hua Gao, MD, PhD
When anti-VEGF therapy is used for treatment of macular edema due to CRVO, it also decreases the rate of neovascular glaucoma.
A Cohort Study of Surgical Transvenous Chorioretinotomies for Macular Edema Due to Retinal Vein Occlusion
Presenter: Jeffrey Luttrull, MD
Chorioretinal anastomoses were done in conjunction with vitrectomy for cases of macular edema due to retinal vein occlusions. This reduced macular edema and also reduced (and in some cases eliminated) the number of intravitreal anti-VEGF injections needed.
